Among the worse outbreaks ever recorded in humankind is the Spanish flu of 1918. This final offensive of the First World War and continuing remarkable episode, this pandemic, swept through the world killing about 3 to as much as 5% of the world’s population, roughly figurers ranging from 50 to 100 million people, within just a year. Notably, although it is known as the Spanish flu, this flu started not in a small country surprisingly situated in Southern Europe.
The War did not suppress any news reporting about Spain as other countries were under strict control. So, it was the first country to expose the Spanish flu. Not only did the Spanish Flue have unprecedented effects on the population around the world, but it equally changed the new management approaches of the public health systems and the world’s attention to the infectious disease evolution aspects.
Origins and Spread of the Spanish flu
It is important to note that the Spanish flu is not a remotely typical disease and its origins continues to be a field of various studies. Some explanations can be directed at Haskell County, in the United States; as that was the place we can hear of an influenza related to extreme strain already in the year 1918, the 1st month in fact.
The outbreak of these initial cases was quite rapid in the military camps and not very surprisingly, Camp Funston in Kansas became the sin center in as far as soldiers infected with the virus went to fight in the World War 1. Yet other theories say that it was in Europe or Asia where the flu virus first began as these regions were some of the first places with outbreaks.
Whatever its source, troop movements in World War I served as a perfect vehicle for the virus’s dissemination to the remotest corners of the earth.
As the year 1918 advanced to spring season, multiple continents had already received the virus. A key differentiator of the Spanish Flu from other common flu pandemics was its fatality levels, as well as its effects on the other age groups, especially the younger people. Seasonal influenza epidemics occur more frequently among the median or older population, as well as vulnerable individuals, however, the Spanish Flu had a different design – 20 to 40 healthy adults became the islands of the illness. This sort of age distribution, combined with the fast and sometimes dangerous course of the illness, was also kulaknij and understanding amazement.
Three distinct waves characterized the Spanish Flu: the first one, the second one and the third one. The initial wave in spring 1918 was the mildest , with comparatively low morbidity increasing with each following season endemicity. Symptoms similar to those of seasonal flu were produced in this wave. This deadly second wave emerged as a result of the complete virulence of the virus onset in the autumn of 1918. It is believed that a change in the virulence and lethality of the virus was the reason for this wave. A third wave was noted in the sophomore quarter of 1919 but it was less rash, however, the cardio-bacterium was practically spent out by that time.
Symptoms and Mortality Rate
The Spanish Flu pandemic was accompanied by one of the most threatening features: the rapidity and certain unusual signs. Patients brought a devastating form of lung inflammation, pneumonia, with accompanying febrile temperatures, cyanosis of the skin or lips, and at times cleeds ouy out of the nares and oral cavity. Some of them died a few hours or few days after the initial complaint of symptoms with some acute respiratory failure. In some instances, the reaction of the immune system was too strong, a cytokine storm, so there was too much swelling and fluid in the lungs contributing to the number of deaths mainly among young adults.
The typical mortality rates have been approximated at about 2-3% in general although observed in some countries, more swathes of segments of the population would get more of the deaths. In insular societies, like some first Nations communities, the rate was catastrophic, sometimes observed up to 90%. The number of deaths across the world during the period of Spanish Flu was made worse due to under feasting, bad situations in which people lived and controlled immunity, especially in Europe where war was rife.
Societal Problems in General and in Healthcare Systems in Particular.
The consequences of the Spanish Flu cannot only be limited to the extraordinary loss of lives. The pandemic also caused disruptions to economies, societies, and healthcare systems on a global scale. Overall public health facilities and materials and Senate both, faced an enormous influx of patients and refugees, sick from appalling wounds received from the war. Hospitals and clinics were severely short on staff and supplies and in many instances, there was insufficient manpower to attend to the ill. In some regions, the entire population was scalped off of doctors and nursing personnel as these fell ill too with no battling from the frontline.
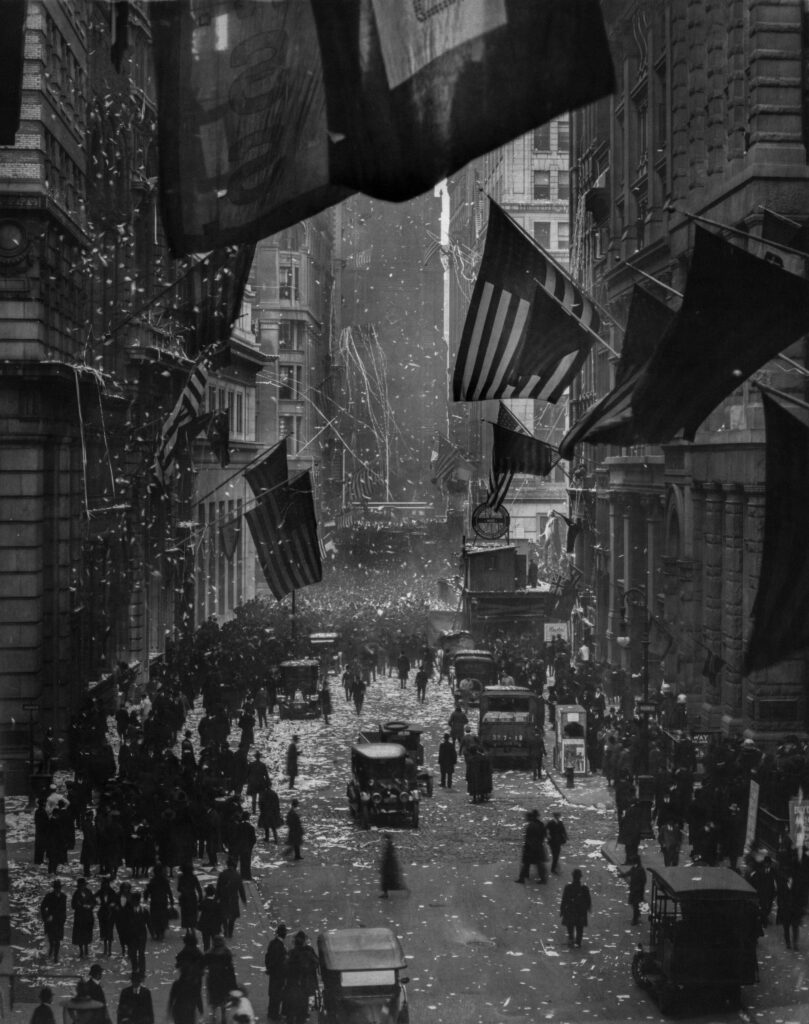
The situation in large metropolitan cities was no better.
Not only where people wearing masks against the risk of getting contaminated by other citizens, but restrictions were also implemented throughout the population. Events where a considerable proportion of citizens gather were banned, schools and church buildings shut down and a good number of companies closed off operations.
The lack of due communication and the censorial policies in several countries only worsened the chaos. As a precaution to use virulent authorities, people had to bear face masks, and isolation was used as well. Nevertheless, as it was realized that the world now faced this changing virus, some failed more so than others as understanding where the infection was coming from was not fully grasped.
The Spanish Flu is memorable also from the economic point of view. Employees got sick or stayed at home to look after sick relatives, factories, businesses, and services ground to a halt. Just as the world was grappling with the fallout of the first war, economies were being brought to stagnation followed by prolonged seasonal recessions due to the pandemic. Furthermore, the massive drain of the pandemic on human life eliminated many workers from the pool and therefore adversely affected the sectors that were crucial to recovery and rebuilding after the war.
The Scientific Response: Medicine begins to turn in response to the force of the problem
Also, the Spanish Influenza pandemic turned out to be an exceptionally important milestone in the history of medicine and public health. Due to the prevailing times, the influenza virus had not yet been unfurled by the scientists and the cause of the pandemic remained to be a mystery. It was not until the decade of 1930 that the researchers were able to separate the influenza virus which paved way for better treatment methods and vaccines in the later time.
Even though modern medicine was not fully available, a few noteworthy developments in public health can be attributed to the Spanish flu epidemic. The concepts of social isolation and isolation of people, sometimes referred to as quarantines, for instance, gained popularity and were seen to be useful in the control of contagious illnesses. The Spanish Flu also contributed to the establishment of many national and global bodies whose functions were and will be the organization of the response to future pandemics, as for instance, the CDC and WHO.
A primary concern during the Spanish Flu pandemic was the absence of many operational modalities of treatment.
There were no antibiotics available to treat consequent infections such as pneumonia, which occurs as a complication of secondary infections. For this reason, numerous individuals who could have overcome the initial viral infection succumbed instead to the subsequent bacterial infections. Managements undergone in those days were the administration of high doses of antipyretic and analgin-acetylsalicylic vitamin – already known aspirin which, however, was clinically very toxic and increased the death rate instead of reducing it.
The pandemic also demonstrated how important rapid and effective communication is in public health. Depending on the right materials, factual, and reliable information was hard to find, forget lead, many communities were already filled with confusion and disbelief in public health leadership. Every person part of the world was taught by the Spanish Flu of 1918. During a pandemic, communicating with citizens fast and honestly helps a great deal in ensuring that order is respected and health guidelines are adhered to.
How World War I Contributed To The Spread Of Spanish Flu
World War I also accelerated the Spanish Flu’s spread and distribution. Soldiers and troopers on the move, as well as being cramped in military tents and barracks, created a favorable environment for the thrive of the virus well into the military milieu. They were as far west as Europe and as far East as Asia, Africa, and North America resulting in viral transport across the pillars of the epidemic stockades. The push for fighting also took away attention and funds from health departments which made the majority of countries vulnerable to the incessant wave of the epidemic attack.
The war also added to the deaths associated with the Spanish Flu. Malnourished, stressed and battered by warfare, those soldiers returned to their homes with greater vulnerability to the disease. In a lot of these cases, these soldiers were the very first ones to bring the virus back to their countries and it spread like wildfire in the general population.
In a way, the Spanish Flu was just as devastating in its effect as the war, as it swept away millions and left many of the surfaces with some health issues. Most of these people had lived through two of the worst preparing revolutions in the course of civilization and this is why the psychological aspect of the disease was of special importance.
Lessons Learned and the Legacy of the Spanish Flu
In many respects, the Spanish Flu was a watershed moment in the evolution of public health policy and the concept of preparedness for pandemics. Although the state of medical science was not sufficiently advanced to provide a solution to the pandemic at that time, it set the stage for enhancing and improving the cooperation to fight diseases in the future.
One of the most important lessons from the Spanish Flu was the recognition of the importance of vaccination. It was in 1918 when such a flu vaccine did not exist that it can be readily found in the market today. The vaccine against these strains of influenza did not become available until the 1940s. Now, millions of people receive flu shots each year, who might otherwise have become victims, in particular, the old and the sick.
The extraordinary investment
That was observed in public health systems as well as the different outbreak detection and response systems were some of the positive impacts brought about by the pandemic. However, the most direct effect of the Spanish influenza pandemic that does not occur with previous outbreaks of influenza pandemic viruses is the establishment of centres for disease control. Such organisations have subsequently been responsible for the rest against the outbreaks of the diseases like HIV/AIDS, SARS, and most recently COVID-19.
The most prominent perhaps of them all is the recognition that a pandemic like this will happen at most anytime with little notice. Otherwise referred to as the 1918 influenza pandemic, the Spanish Flu was also a great teacher of the weakness of man faced with contagious diseases, a mitigating lesson whose effects are still being felt to date especially with the Coivd-19 still around. The health authorities continue to make the same arguments that action should be taken to minimize the danger to public health that such future pandemics might bring.
Comparison with the SARS-COV2 Pandemic
The COVID-19 pandemic that began in the winter of 2019-20 has been called the second coming of the Spanish flu pandemic that struck in 1918-19. These pandemics were catastrophic in that they affected virtually the entire populations of the world and strained the available medical resources with a slight margin of exception. Once again, people faced the difficult question of how to treat, and yes, vaccinate, people against such an enigmatic problem as a pandemic.
Nevertheless, the two pandemics can also be construed preventably) distinctly different. As compared to other historical pandemics and epidemics, Sars-COV2 pandemic responses have been efficient due to improved levels of public health, information, and medicine. The rapidity of the protection of all vulnerable people by vaccination and technological capacity such as tracking down cases did not occur in the Spanish flu period.
Correspondingly, the healthcare systems would have to make adjustments to the societal changes caused by the diámetro of canales por años.



Pingback: The Importance of Sleep Hygiene: Key Habits for Better Sleep - healthyplusorigin